ABSTRACT: 0007
Establishing Oral-Systemic Linkage Profiles Using Matrix Analyses of Relative-Risk Correlations
| R. LEE, New York University College of Dentistry, USA, and R. LEVINS, Harvard School of Public Health, Boston, MA, USA |
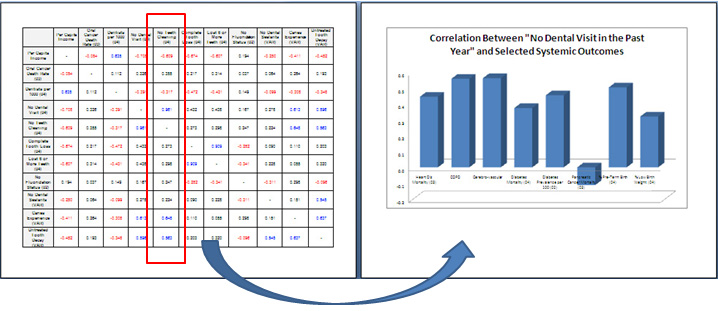
OBJECTIVES: Emphasis on oral-systemic linkages by prominent health-policy publications like Health People 2010 and Oral Health in America: a Report of the Surgeon General has invigorated inquiry into the physiological/biochemical models between oral and systemic outcomes. To date, however, no study has corroborated such oral-systemic linkages using matrix-analyses of correlations using federal-level (e.g. CDC, NHANES) data. We 1) examined whether said linkage profiles (e.g. periodontitis and heart disease) can be established using matrix-analyses of relative-risk correlations and 2) identified positive and negative oral health indicators with most significant relationships to various systemic conditions. METHODS: We examined correlation trends between the fifty states (and District of Columbia) in a) general demographic indicators; b) positive oral-health indicators; c) negative oral-health indicators; d) oral behaviors/conditions implicated in systemic diseases and; e) systemic conditions caused by oral behaviors/conditions, and used matrix analyses to establish oral-systemic linkage profiles. RESULTS: Systemic outcomes including “heart disease mortality,” “diabetes prevalence” and “% pre-term birth” showed relatively significant negative correlations to positive oral health indicators (e.g. “dentists-per-1000), verifying oral-systemic linkage profiles. In contrast, “pancreatic cancer mortality” showed a positive relationship, indicating the lack of a clear oral-systemic linkage. With negative oral health indicators (e.g. “%-of-population-without-a-dental-visit-in-the-past-year”), heart disease, COPD, cerebrovascular disease, pre-term birth, and low-birth weight all implied positive correlations, thus establishing an oral-systemic linkage profile, while others like “no-fluoridation-status” and “%-population-without-a-dentist-in-the-entire-county” failed to show clear directionality. Smoking and adult/childhood obesity indicators were some of the strongest oral behavior/condition indicators implicated in systemic diseases, while alcohol and smokeless tobacco use showed weaker correlations. CONCLUSIONS: Variability in systemic health relative risks reflects differences in selected oral health indicators and their impact on overall health. The directionality of correlations of relative risks of selected oral and systemic health indicators helps establish linkage profiles and may point to areas of further investigation. |
| Seq #6 - Oral and Systemic Health 3:15 PM-4:45 PM, Wednesday, April 2, 2008 Hilton Anatole Hotel Senators Lecture Hall |
|
Back to the Behavioral, Epidemiologic, and Health Services Research Program |
©Copyright 2008 American Association for Dental Research. All Rights Reserved.